It was the waiting that first taught him about healthcare in this country.
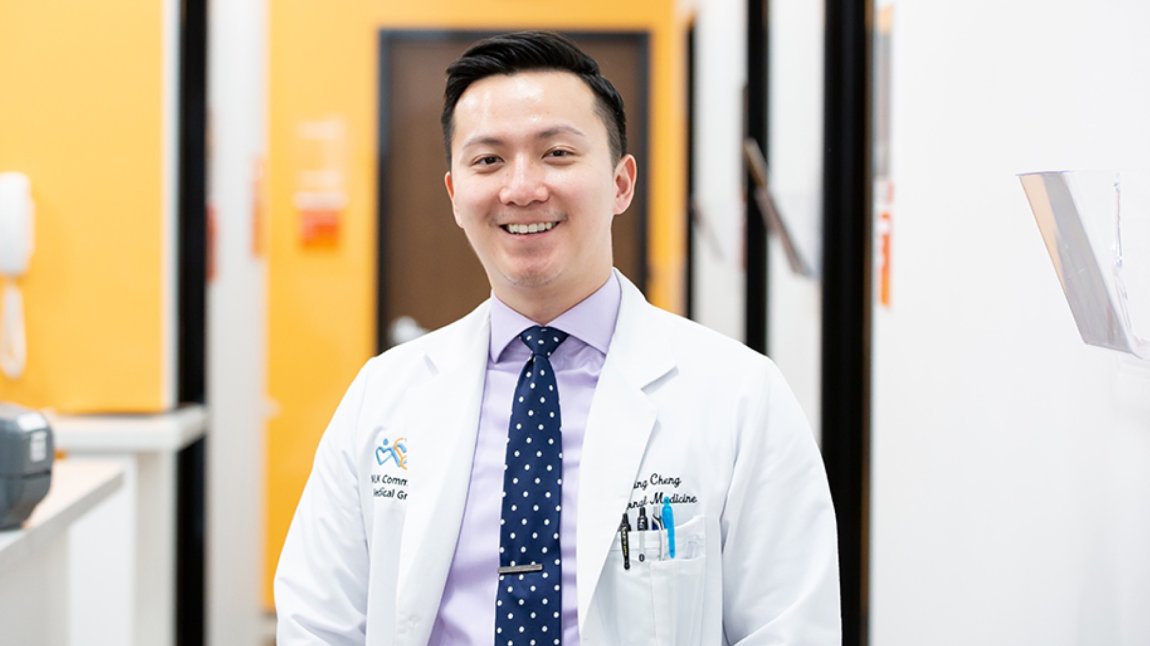
For two hours, twelve-year-old Ben Cheng sat with his immigrant parents in an overcrowded waiting room. They were there to see one of the few doctors who spoke their language and would treat those like his family: low-income, immigrants, and covered by Medicaid, the lowest-paying form of public insurance.
Two hours to see a doctor, two hours of staring at the blank walls and cracked linoleum. Children wove through the crowded room, but the adults sat quietly. They had grown used to the wait.
It was the early 1990s and Ben Cheng’s parents had already left behind two homes in search of a better life. From their hometowns in China’s Fujian Province they moved to Hong Kong, where Ben was born. Their search eventually took them to New York City’s Chinatown.